December 18, 2020
The McKnight Endowment Fund for Neuroscience has selected three projects to receive the 2021 Neurobiology of Brain Disorders Awards. The awards will total $900,000 over three years for research on the biology of brain diseases, with each project receiving $300,000 between 2021 and 2024.
The Neurobiology of Brain Disorders (NBD) Awards support innovative research by U.S. scientists who are studying neurological and psychiatric diseases. The awards encourage collaboration between basic and clinical neuroscience to translate laboratory discoveries about the brain and nervous system into diagnoses and therapies to improve human health.
“It’s exciting to have the opportunity to support some of the nation’s leading neuroscientists in their trailblazing research,” said Ming Guo, M.D., Ph.D., chair of the awards committee and Professor in Neurology & Pharmacology at UCLA David Geffen School of Medicine. “This year’s awardees are conducting research into issues that affect huge numbers of people and society as a whole: Parkinson’s Disease, migraines, and the epidemic of chronic pain that underlies the opioid crisis. By understanding the underlying neurobiology of disease propagation and how these brain disorders operate at the network and cellular level, we open the door to new ways to prevent, minimize, and treat them.”
The awards are inspired by the interests of William L. McKnight, who founded The McKnight Foundation in 1953 and wanted to support research on brain disease. His daughter, Virginia McKnight Binger, and the McKnight Foundation board established the McKnight neuroscience program in his honor in 1977.
Multiple awards are given each year. This year’s three awardees are:
- Rui Chang, Ph.D., Assistant Professor, Departments of Neuroscience and of Cellular and Molecular Physiology, Yale University School of Medicine; and Sreeganga Chandra, Ph.D., Associate Professor, Departments of Neurology and Neuroscience, Yale University School of Medicine, New Haven, CT
From gut to brain: Understanding the propagation of Parkinson’s Disease: Dr. Chang and Dr. Chandra aim to uncover how Parkinson’s Disease propagates from the gut to the brain via the vagus nerve and to explore ways to slow or inhibit this spread. - Rainbo Hultman, Ph.D., Assistant Professor, Department of Molecular Physiology and Biophysics, Iowa Neuroscience Institute – Carver College of Medicine, University of Iowa, Iowa City, IA
Brain-wide electrical connectivity in migraine: Toward the development of network-based therapeutics: Dr. Hultman’s research will create a brain-wide map of the electrical activity present in migraines and test the effect of therapeutics on this activity. - Gregory Scherrer, Ph.D., Associate Professor, Department of Cell Biology and Physiology, UNC Neuroscience Center, University of North Carolina, Chapel Hill, NC
Elucidating the neural basis of pain unpleasantness: Circuits and new therapeutics to end the dual epidemic of chronic pain and opioid addiction: Dr. Scherrer’s work focuses on uncovering how neurons in the brain process pain information as a first step to find new and better ways to relieve chronic pain suffering without the negative side effects of many common painkillers.
With 87 letters of intent received this year, the awards are highly competitive. A committee of distinguished scientists reviews the letters and invites a select few researchers to submit full proposals. In addition to Dr. Guo, the committee includes Sue Ackerman, Ph.D., University of California, San Diego; Susanne Ahmari, M.D., Ph.D., University of Pittsburgh School of Medicine; Robert Edwards, M.D., University of California, San Francisco; Andre´ Fenton, Ph.D., New York University; Tom Lloyd, M.D., Ph.D., Johns Hopkins Medical School; and Harry Orr, Ph.D., University of Minnesota.
Letters of intent for the 2022 awards are due by March 15, 2021.
About the McKnight Endowment Fund for Neuroscience
The McKnight Endowment Fund for Neuroscience is an independent organization funded solely by the McKnight Foundation of Minneapolis, Minnesota, and led by a board of prominent neuroscientists from around the country. The McKnight Foundation has supported neuroscience research since 1977. The Foundation established the Endowment Fund in 1986 to carry out one of the intentions of founder William L. McKnight (1887–1978), one of the early leaders of the 3M Company.
The Endowment Fund makes three types of awards each year. In addition to the Neurobiology of Brain Disorders Awards, they are the McKnight Technological Innovations in Neuroscience Awards, providing seed money to develop technical inventions to advance brain research; and the McKnight Scholar Awards, supporting neuroscientists in the early stages of their research careers.
2021 NBD Awards
Rui Chang, Ph.D., Assistant Professor, Departments of Neuroscience and of Cellular and Molecular Physiology, Yale University School of Medicine
Sreeganga Chandra, Ph.D. Associate Professor, Departments of Neurology and Neuroscience, Yale University School of Medicine
From gut to brain: Understanding the propagation of Parkinson’s disease
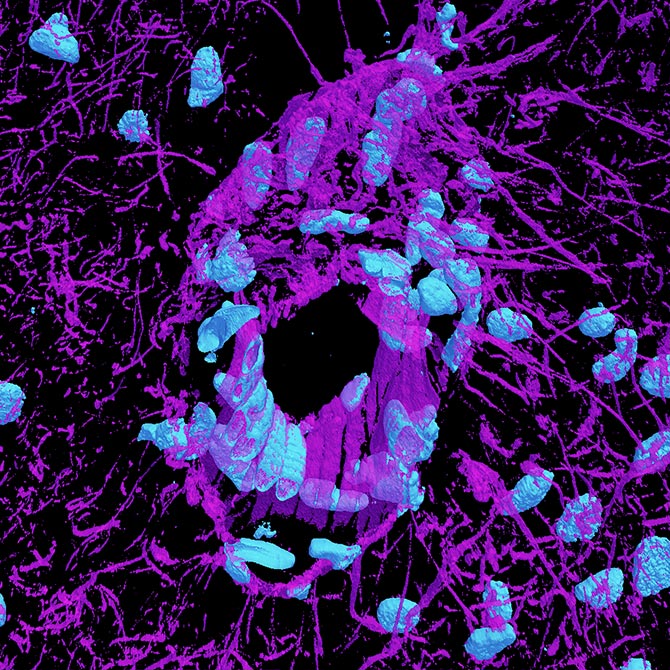
Parkinson’s Disease is a widely known but still mysterious neurological degenerative disease that dramatically affects quality of life. Exactly how the disease initiates is unknown, but recent research indicates that at least some Parkinson’s cases originate in the gut and propagate to the brain via the vagus nerve, a long, complex, multifaceted nerve connecting many organs to the brain.
Dr. Chang and Dr. Chandra are taking this gut-to-brain propagation insight to the next level with their research. Their first two aims seek to identify exactly which vagal neuron populations transmit Parkinson’s and the process by which the gut and these neurons interact. The experiment uses a mouse model, injections of proteins that can induce Parkinson’s, and a novel process to tag and selectively ablate (shut down) specific types of neurons. Through experiments in which certain neurons are ablated, the protein introduced, and the mice examined for Parkinson’s, the team will narrow in on specific candidates. In the third aim, the team hopes to uncover the mechanism by which the disease is transported at the molecular level within neurons.
The research is a collaborative, interdisciplinary effort drawing upon Dr. Chang’s experience researching the vagal nerve and enteric system and Dr. Chandra’s expertise in Parkinson’s Disease and its pathology. It is hoped that with a better, more precise understanding of how the disease reaches the brain, new targets farther from the brain can be identified for treatment that are more precise, allowing treatment to delay or diminish the onset of Parkinson’s without harming the brain or affecting the many other important functions of the extraordinarily complex vagal nerve or the enteric system.
Rainbo Hultman, Ph.D., Assistant Professor, Department of Molecular Physiology and Biophysics, Iowa Neuroscience Institute – Carver College of Medicine, University of Iowa
Brain-wide electrical connectivity in migraine: Toward the development of network-based therapeutics
Migraine is a widespread, often debilitating disorder. It is complex and notoriously difficult to treat; sufferers have differing symptoms, often triggered by sensory hypersensitivity, that may include pain, nausea, visual impairment, and other effects. Migraine affects multiple interconnected parts of the brain, but not always in the same way, and treatments often won’t have the same effect from person to person. Dr. Hultman’s research proposes to examine migraines using new tools with the aim of illuminating new paths for treatment.
The research builds upon her team’s discovery of electome factors, measurements of electrical activity patterns in the brain tied to specific brain states. Using implants to measure brain activity in mouse models representing both acute and chronic migraine, her team will observe which parts of a mouse brain are activated and in what sequence on a millisecond scale for the first time. Machine learning will help organize the collected data, and the electome maps created can be used to help identify the parts of the brain affected, and how the electome changes over time, particularly through the onset of chronicity. The experiment also examines electrical activity patterns tied to behavioral response; for example, the electrical signals observed in the brain of a subject who seeks to avoid bright lights may offer a way to predict more severe responses to migraine.
A second part of Dr. Hultman’s research will then use the same tools to look at how available therapeutics and prophylactics work. Electome factors of subjects treated with these therapeutics will be collected and compared with controls to identify what parts of the brain are affected and in what way, helping reveal the effect of each therapeutic/prophylactic, as well as the effects of medication overuse headache, a common side effect experienced by migraine sufferers who seek to manage their condition.
Gregory Scherrer, Ph.D., Associate Professor, Department of Cell Biology and Physiology, UNC Neuroscience Center, University of North Carolina
Elucidating the neural basis of pain unpleasantness: Circuits and new therapeutics to end the dual epidemic of chronic pain and opioid addiction
Pain is how our brain perceives potentially harmful stimuli, but it’s not a single experience. It’s multidimensional, involving transmissions from nerves to the spinal cord and brain, processing of the signal, triggering of reflexive action, and then follow-up neural activity involved in actions to soothe the pain in the near term and complex learning processes to avoid it in the future.
Pain is also at the core of what Dr. Scherrer sees as two interrelated epidemics: the epidemic of chronic pain, affecting some 116 million Americans, and the opioid epidemic that results from the misuse of powerful and often addictive drugs to treat it. In his research, Dr. Scherrer is looking to find out exactly how the brain encodes the unpleasantness of pain. Many drugs seek to affect that sense of unpleasantness but are often overbroad and also trigger the reward and breathing circuits, leading to addiction (and by extension overuse) and the respiratory shutdown responsible for opioid-related deaths.
Dr. Scherrer’s team will generate a brain-wide map of pain emotional circuits using genetic trapping and labelling of neurons activated by pain with fluorescent markers. Second, activated brain cells will be separated out and their genetic code will be sequenced, looking for common receptors on those cells that may be targets for therapeutics. Finally, the research will investigate compounds in chemical libraries designed to interact with any of those identified target receptors; the effects those compounds have on the unpleasantness of pain; and whether these compounds also carry risk of overuse or affect the respiratory system. Ultimately, the intention is to help find better ways to relieve all types of pain and to improve the well-being and quality of life of patients who experience it.